Clinical Trials for Investigational Products
As researchers, our work is focused on developing science into cutting-edge therapies. What we do today may improve the lives of people tomorrow. One crucial part of developing innovative therapies and making them available to the public are clinical trials, carefully supervised research that evaluates the safety and efficacy of investigational products in humans. We aim to improve, extend, and potentially save lives with our research.
BioNTech Clinical Trials
We are currently advancing more than 25 product candidates in the field of cancer and infectious diseases.

Clinical Trial Design
Clinical trials are a crucial part of the drug development process. They are research studies involving human volunteers and are conducted to investigate whether a new therapy, vaccine, or medical device is safe and effective in humans. They can also be performed to evaluate a new way of using an existing treatment or evaluate a combination of drugs for a single disease.
As clinical trials involve humans, they are carefully designed and extensively monitored, and they are required to be approved by the appropriate regulatory authorities, as well as by independent ethics committees (IECs) or review boards (IRBs), before they can start. Clinical trials may be conducted at multiple sites, for example a hospital or clinic, and in different regions within a single country as well as in multiple countries. Geographic location plays an important role in conducting our clinical studies to help ensure that trial participants are representative of the population that will benefit from the treatment. Before a novel product candidate can be approved, it must complete a rigorous clinical development process, which includes several phases.

Phases of Clinical Trials
The development of novel treatments is a comprehensive and strictly structured research process that is done in several steps, so-called “phases”. Each phase is designed to answer certain questions about the investigational product being tested while aiming to keep the participants in each trial as safe as possible. The trial designs in each phase can differ widely, depending on whether the trial evaluates product candidates for disease prevention (e.g., prophylactic vaccines against flu) or product candidates that treat medical conditions (e.g., cancer). Depending on the trial objectives, healthy volunteers or patients may participate in the trial.

Preclinical
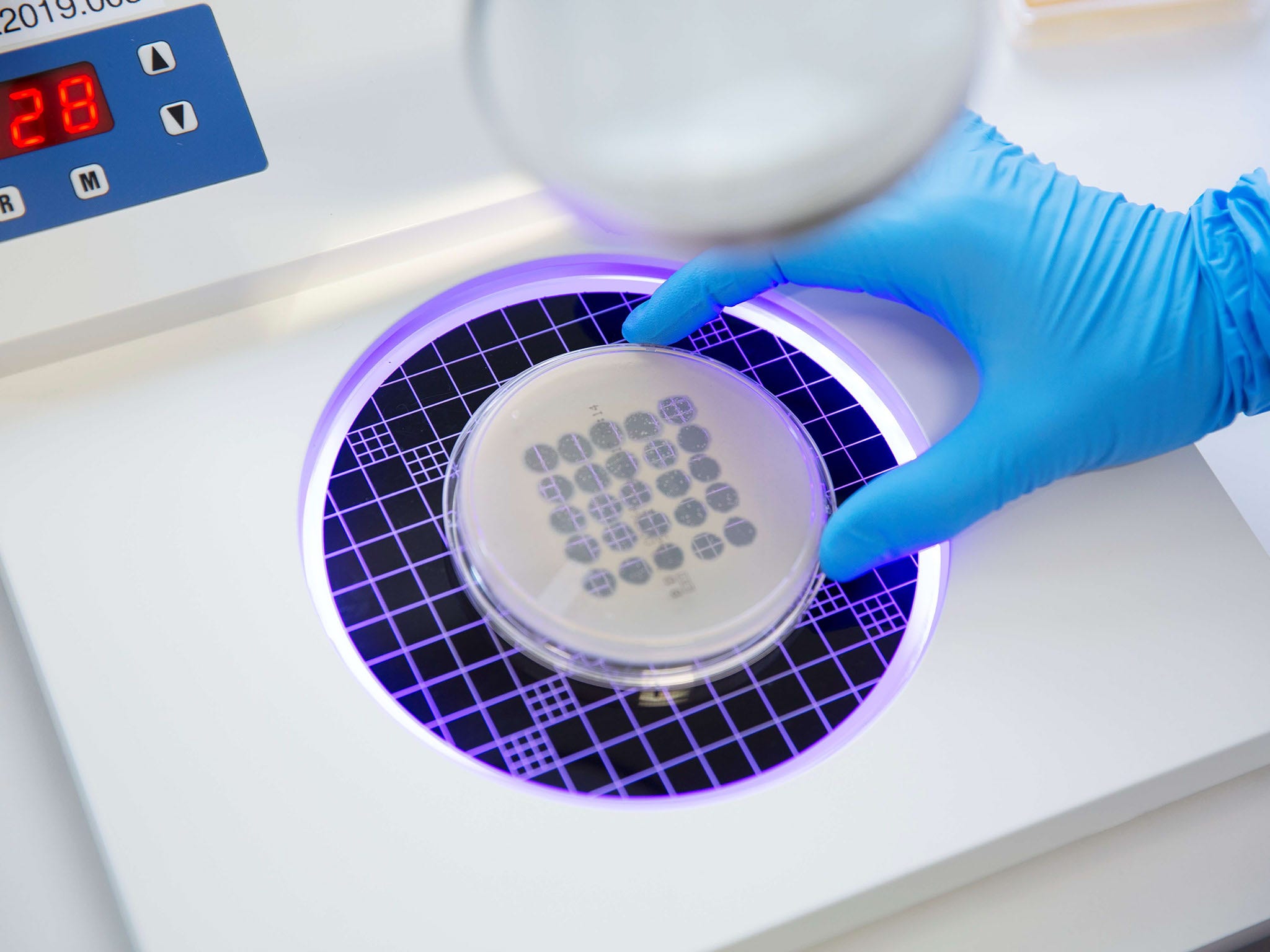
Before an investigational product can enter clinical trials in humans, potential candidates are studied by researchers in the laboratory. The “preclinical phase” includes a number of lab studies which are conducted to evaluate if the new treatment is potentially safe and effective to be tested in humans.

Phase 1
Phase 1 clinical trials are generally conducted in a small number of individuals, up to a few dozen per treatment. The main goal of this phase is to assess the product candidate’s safety and tolerability. This includes finding the highest acceptable dose of the product candidate. A secondary goal is to evaluate the effects of the product candidate on the body and what happens to the product candidate once administered. During clinical trials, trial participants are closely monitored for side effects following the administration of the product candidate. If an acceptable safety profile is shown, the product candidate can enter a Phase 2 clinical trial.
If the trial is placebo-controlled, both the attending physician and the trial participants may be blinded, which is called a double-blinded trial. This means that neither the attending physician nor the trial participant know what treatment the participant receives. In some Phase 1 trials, only the trial participant may be blinded. Blinding allows the effect of the treatment versus the placebo to be better evaluated.

Phase 2
Phase 2 clinical trials are designed to study the safety and tolerability of the product candidate in a larger group of individuals (usually up to 100 per treatment), and to evaluate the early efficacy of the product candidate in the target population. Multiple Phase 2 trials can be conducted to study the product candidate in different patient populations or disease indications. If it is a placebo-controlled trial, the Phase 2 trial can be blinded to the attending physician and/or the participating individuals. For indications in oncology, the Phase 2 trials may be open-label, i.e., the attending physician and the trial participant know what treatment the participant receives. In some instances, the trial participants are randomized, meaning that the participants are randomly assigned to different treatment groups. This randomization reduces potential bias when comparing the effect of different treatments. Phase 2 trials help define the product candidate treatment regimens (the dose, the dosing frequency, and the duration of dosing) for use in Phase 3 trials, which prove the safety and the efficacy of the investigational product.

Phase 3
Phase 3 clinical trials are conducted in a large group of individuals (up to several hundreds or thousands per treatment) and in different regions or countries, to prove that a product candidate is safe and efficacious in the patient populations or disease indications for which it is being assessed. As these trials usually have a much larger number of trial participants and much longer observations periods, they are more likely to detect possible rare or long-term side effects. In most instances, the Phase 3 trials compare the product candidate with the current standard of care, if available. Some Phase 3 trials also study the product candidate in combination with other authorized therapies. Information from Phase 3 trials is usually the basis for requesting marketing authorization.

Phase 4
Phase 4 clinical trials are conducted after the investigational product is approved by regulatory authorities. These trials continue to assess the safety and efficacy of the new drug along with its long-term effects in a real word setting. They may take place over many years and usually involve a large number of participants.
Combined phase clinical trials
In cancer drug development, clinical trials can also start in patients in a combined Phase 1 and Phase 2 clinical trial, referred to as Phase 1/2, if the investigational product and the medical need meet certain criteria. This form of clinical trial simultaneously evaluates the safety as well as early signs of efficacy of the investigational product. Combined phase clinical trials – both Phase 1/2 and Phase 2/3 – can also occur in other disease indications or during vaccine development.

Frequently used terms in a clinical trial
Every clinical trial follows strictly defined protocols and assesses defined clinical outcomes. Learn more about the terminology here
